Medical Claims Processor | Data Analyst
• Entering client and account data from source documents accurately.
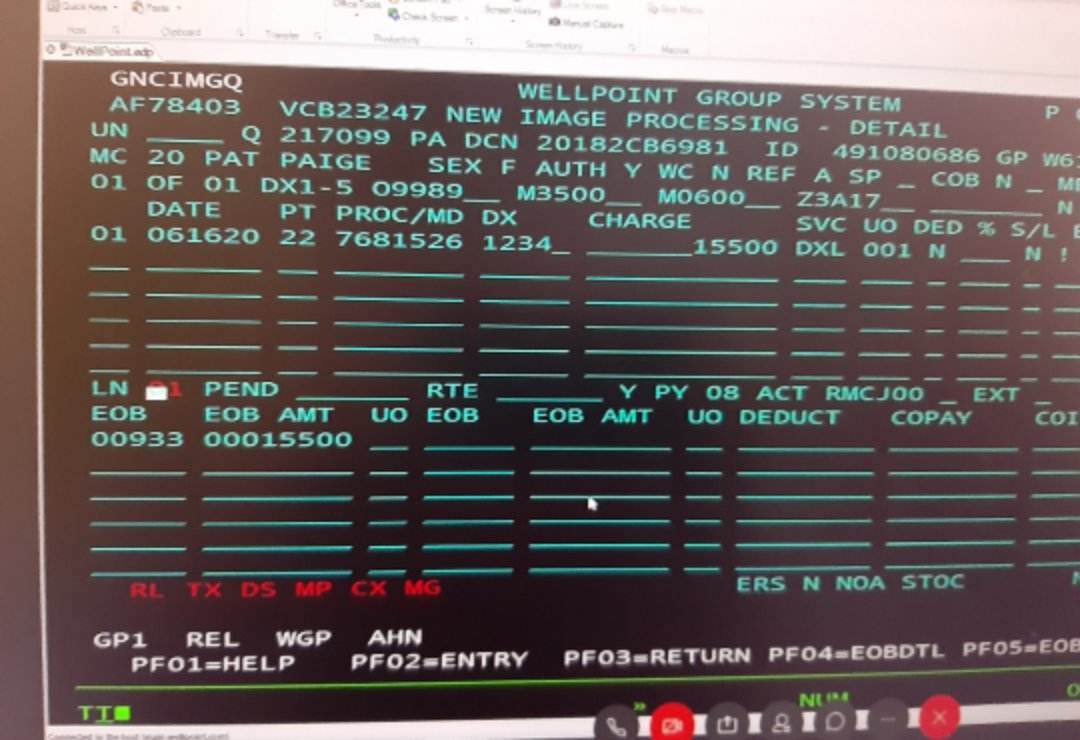
• Review claim submissions, obtain and verify information, correspond with insurance agents and beneficiaries, and process claim payments.
• Compiling, verifying accuracy, and sorting information to prepare source data for computer entry.
• Knowledgeable in medical coding and health care cost sharing
• Process claims with different US health insurances like Anthem, BCBS, CIGNA, AETNA
• Trained to comply HIPAA guidelines/regulations
• Authorize to disclose information such as claim denial and status after HIPAA
• Review claim payments and allowed amounts if underpaid or overpaid •
Scan documents received from providers like medical records, appeal, pre auth
• Verify patient’s claims, benefits and eligibility, pre-certification requirement
• Determine correct coordination of benefit for health claims


